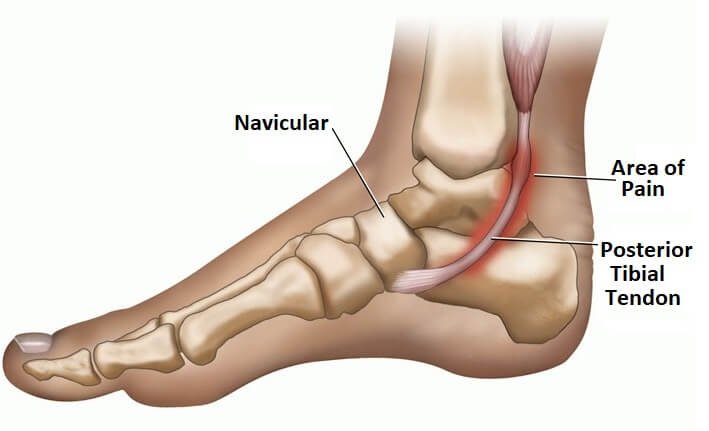
Posterior Tibialis Tendonitis
The posterior tibial tendon is not well known, but it is hugely important to the stability of your foot. Not much thicker than a lead pencil, this tendon along with the Tibialis Posterior muscle, applies tension along the inside of your ankle in a way that stabilises and supports the arch of your foot. Without this function, your foot will flatten and loose its spring loading.
Posterior Tibial Tendon dysfunction is a disorder causing progressive weakening and loss of strength of the tendon. As a result, the tendon may not be able to provide stability and support for the arch of the foot. This results in a flatfoot that can be painful along the inside of the foot. Although it is not a common issue, if it remains untreated, the bearer may be left with a permanently deformed foot.
Symptoms
· sharp pains in your arch (side) or foot
· visible inflammation along the tendon
· stiffness in your ankle joint
· a popping sensation
· soreness to the touch
· difficulty or inability to walk or run due to the resultant pain
Causes
Genetics: Structural alignment of bones within the foot is predominantly inherited, so having high arched feet is generally inherited from parents or grandparents.
Disease: In some instances, neuromuscular diseases can cause high arched feet. For example; Charcot Marie Tooth Syndrome
Treatment Options
Ice
Treatment in the first 48–72 hours of injury to reduce bleeding, swelling and inflammation. R.I.C.E regime comprises of rest from activities, crutches may be needed, regular icing, use of a compression bandage and elevation of the limb.. Apply cold packs on the most painful areas for 20 minutes at a time, 3-4 times daily to keep down swelling. Do not apply ice directly to the skin. Anti-inflammatory medication may be useful in the early phase to help the healing process by reducing swelling and pain.
Rest
Pain may last longer than 3 months even with early treatment. For patients with a chronic condition, it is not uncommon for the pain to last another 6 months after treatment starts. Decrease or stop activities that increase pain. Switch to low-impact exercise. Biking, use of elliptical machines and swimming have less impact on the foot and are more tolerable. Placing ice over the tendon immediately after the cessation of exercise helps to decrease inflammation around the tendon. We provide further education on pain-free movements and strengthening and balance exercises to do early in the rehabilitation process to prevent stiffness and muscle weakness, to ensure the foot and ankle are functioning correctly.
Nonsteroidal Anti-inflammatory Medication
Drugs, such as ibuprofen or naproxen, reduce pain and inflammation.
Taking medication about 30 minutes prior to exercise rehab helps limit inflammation around the tendon. Any thickening that is present, is degeneration of the tendon and it won’t go away with medication. Be sure to talk with your GP if these medications are needed for more than one month.
Immobilization
A short-leg cast or walking boot may be used for 6 to 8 weeks. This allows the tendon to rest and the swelling to subside. A cast causes other muscles of the leg to atrophy (decrease in strength) and thus is only used if the more conservative treatments do not work.
Orthotics
Most people can be helped with orthotics or braces. It is the common non-surgical treatment for flat feet.
Buying a prefabricated device may be enough if the change in the shape of the foot is mild. But custom orthotics are needed if changes in the shape of the foot are moderate to severe. It may be more costly, but it allows for better control in the position of the foot.
Whatever is needed in your case can advised by a podiatrist.
Braces
A lace-up ankle brace may be helpful with a mild to moderate flatfoot. The brace will support the joints of the back of the foot and take tension off of the tendon. A custom-moulded leather brace is needed in severe flatfoot where the foot has b eco me stiff or arthritic. The brace can help some patients avoid surgery.
Physical Therapy
Physical therapy that strengthens the tendon can help with mild to moderate disease of the posterior tibial tendon.
Steroid Injection
Cortisone is a powerful anti-inflammatory medicine that your doctor may consider injecting around the tendon. A cortisone injection into the tendon is not normally done, because it carries a risk of tendon rupture. Discuss the full implications before getting any injections.
Remember, you are dealing with a condition that may jeopardize your future mobility. It may also develop a permanent foot deformity, so commit to the treatment regime fully.
Answering your questions and concerns about the high arches is important to MyFamilyPodiatrist. We want you to be in the best position to actively address the issues and support healthier foot function.
Whatever approach is needed to improve your mobility, it will be a shared journey between you and our podiatrist, with your wellbeing central to the process..
Contact us on admin@myfamilypodiatrist.com.au
Take the first step!